Questions for My Doctor in English + 16 Additional Languages
Questions You Can Ask Your Care Team About Lobular Breast Cancer
As you explore this website, you will have an opportunity to learn about invasive lobular carcinoma (ILC), also known as lobular breast cancer. It is the Lobular Breast Cancer Alliance’s (LBCA) intention to provide information for you to consider when making decisions. It is our hope that the knowledge you gain from our website, and from perhaps using some of these questions with your doctors, will help you better understand your circumstances and become more comfortable talking with your care team.
We prepared these questions to be used with various members of your care team or with someone from whom you may be seeking another opinion. In preparing the questions, we have developed this resource with the input of patient advocate volunteers as well as clinicians on our Scientific Advisory Board (SAB). We recognize that everyone is unique, and cancer is a complex disease. We also reiterate that not all lobular breast cancers are the same. Cancers vary in genetic makeup. Everyone has different medical histories, co-occurring illnesses, lifestyles, and social supports. Your doctors take all these factors into consideration in your diagnostic work-up, treatment plan, and in monitoring your ongoing care. Therefore, we offer these questions with the understanding that they may not all apply in your case.
(Published 3/21/2023)
View and download the Questions For My Doctor document in other languages:
We have grouped the aforementioned questions in English into categories so that you may read and/or print out all or only those most relevant for you. Questions in Section 1 pertain to individuals with all stages of ILC while Sections 2 and 3 pertain specifically to metastatic ILC.
(Published 3/21/2023)
Section 1: Questions Pertaining to ILC – All Stages
- Are you a breast cancer specialist?
- How familiar are you with treating patients with lobular breast cancer? Who else will be on my team?
- Are you familiar with the current research on lobular breast cancer? Are you open to me sharing with you any new studies or research I may come across?
- Are you comfortable with me seeking a second opinions if I choose to do so?
- How large is the tumor(s)
- Does the imaging show more than one tumor in the breast? If so, are the other tumors in the same quadrant of my breast? Are there any in the other breast?
- Do you recommend an ultrasound or MRI to supplement the mammogram? What additional information can these tests provide?
- Can you feel the tumor? Can you measure it? Can you show me where it is/they are?
- Do you feel any large or suspicious lymph nodes in my armpits? Are suspicious nodes seen on any imaging test?
- Will I need a biopsy? What type of biopsy do you recommend? What will the biopsy reveal? Will the biopsy reveal anything about lymph node involvement? How is the biopsy done?
- What tests confirm that I have lobular breast cancer?
- What does classic or non-classic lobular breast cancer mean?
- Did you test the tumor to determine if it is Estrogen receptor positive (ER+)? Progesterone receptor positive (PR+)? HER2 positive or Triple negative [1] (TNBC)? If it is ER+ or PR+, how strong is the positivity? What is the significance of these results for me and my treatment? What do IHC (immunochemistry) tests mean and what do the results indicate?
- I understand that Ki67 measurement is not done routinely but when is Ki67 measured?
- There is molecular subtyping luminal A and luminal B. What does that mean?
- What is the cancer stage? How is this determined?
- What is the tumor grade and what does it mean?
- What do these measurements mean and how will these results guide the treatment you recommend?
[1] Triple negative is rare in cases of ILC.
- Are there more tests that I need, such as an MRI or CT or PET scan or bone scan to see if the cancer has spread outside of the breast?
- How does lobular breast cancer affect your decision about what other imaging tests to order?
- Do you plan on sending a specimen for Oncotype DX or MammaPrint or other prognostic or predictive testing? Why/why not? How will these results affect my treatment options?
- Do you recommend genetic testing? If so, what will you test for (BRCA1, BRCA2, CDH1, or other hereditary mutations)? Why/why not? When should this happen? Is there a genetic counselor in this practice/clinic/center with whom I can meet?
- How will this information be useful in your treatment recommendations and my care plan decisions?
- If I am BRCA positive – please explain to me under what circumstances you will recommend a mastectomy and/or oophorectomy (ovary removal), what my other options are and what difference in long term survival will these different options make?
- If I have a different germline mutation (i.e., an inherited genetic mutation) such as the ATM gene mutation, how will this impact my care?
- Are you recommending surgery, radiation therapy, and/or systemic therapy (hormonal or chemotherapy or both)? Please explain the reasons for this proposed treatment plan.
- In what order will these treatments occur? Who should I talk with about the side effects of these treatments when I am going through them if I experience them?
- Will you recommend other lifestyle or nutritional changes? Will you want me to take calcium or vitamin D or any other supplements? Is there a nutritionist and/or exercise program in your practice/facility or in the area that you recommend?
- Why are you recommending chemotherapy?
- Will I need the chemotherapy before or after my surgery? What is the reason for the proposed timing? Which chemotherapy are you recommending for me and why?
- Will I need any additional tests (such as a test to check my heart function) before I start chemotherapy?
- What are the side effects of the chemotherapy you are recommending? What remedies will there be for avoiding or minimizing side effects?
- Can cold caps or something else minimize my hair loss?
- Is there someone I can speak with about how to get a wig? Are wigs generally covered by insurance?
- Will I need a port? Can we discuss the pros and cons of a port?
- What else do I need to know about the chemotherapy you propose including? And what other resources and supports do you recommend?
- Which hormonal therapy are you recommending and why?
- When will I start the hormonal therapy? Will I wait until after radiation or chemotherapy?
- How is my menopausal status factored into this decision? If I am pre-menopausal, what will you recommend and why? Am I a candidate for an oophorectomy or other types of ovarian suppression? If I am a candidate for oophorectomy, when would I have this procedure?
- How long are you recommending that I have hormonal therapy? Can you explain how hormonal therapy reduces my risk of recurrence and whether my risk is reduced further depending on how long I remain on the hormonal therapy?
- What are the side effects I can expect? Who should I talk to about the side effects? Should I expect the intensity of side effects to change over time? Is there an option for switching hormonal treatments or lowering the dose if the side effects are too great? Is there an option for a hormone therapy holiday?
- Can you explain any potential negative effects the hormone therapy options can have on my bones, heart, weight, and the risk of developing other cancers?
- Should I have a bone density test? If I already have osteoporosis or osteopenia, will you recommend bisphosphonates or other bone strengthening agents due to risks of increased bone loss from some anti-estrogen drugs? Will your recommendation be different if I am going to be taking Tamoxifen vs. an aromatase inhibitor? If recommended, how often will I need to take them and for how long? If there are different options for how they can be administered can you explain the advantages/disadvantages of each including if one or more option won’t be covered by insurance?
- If I will be taking bisphosphonates, what are the risks of ONJ (Osteonecrosis of the jaw)? What are the other side effects? I have heard that they can cause problems with dental work, can you explain? Will I need to stop taking them for any dental work?
- How will you follow me after treatment? Will I need to get routine blood tests or check-ups or scans? How often?
- What type of imaging will you recommend and how often? Do you recommend that I be followed with MRIs in addition to mammograms?
- What is my risk for recurrence? How long do you recommend that I take the prescribed treatment to prevent recurrences?
- What are the risks of metastatic spread? How long will you follow me for?
- What are likely places the cancer could recur?
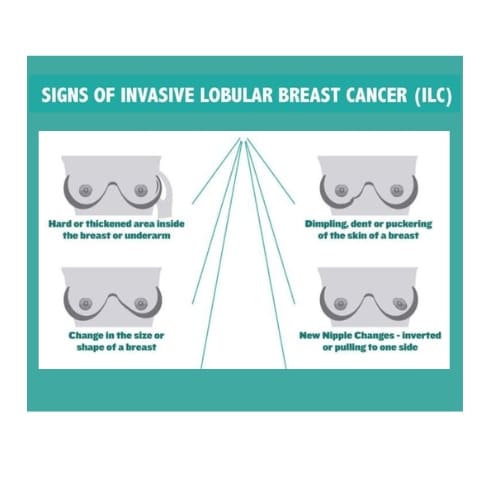
- What signs or symptoms of possible recurrence or metastasis should I bring to your attention?
- Should I continue doing breast/chest self-exams and checking under my arms for swollen nodes?
- Do you specialize in breast cancer?
- What is your experience with surgery in patients with lobular breast cancer?
- Do you recommend a lumpectomy or a mastectomy for me? What are the risks and benefits of each?
- If the tumor is large, do you recommend shrinking it with chemotherapy or hormonal therapy first to make it easier to clear the margins? Approximately how long will this take? Are there any risks involved in waiting for surgery?
- If you are recommending a lumpectomy, do you think you can achieve clear margins in my case? If you cannot obtain clear margins the first time, will you recommend a second lumpectomy? Under what circumstances would you recommend that I have a mastectomy after a lumpectomy?
- If I have a lumpectomy, will I necessarily need radiation? Can I avoid radiation by having a mastectomy?
- What technique do you use to locate the tumor and lymph nodes before surgery?
- How will you determine whether the margins are clear?
- What techniques do you use to obtain clear margins? Does the hospital I will be in have the capacity to test in the operating room if my surgeon has not obtained clean margins and allow him/her to do an additional excision immediately?
- Are you familiar with Oncoplastic technique? Is Oncoplastic lumpectomy an option for me? Oncoplasty may be useful in ILC because you can remove more tissue in order to obtain clear margins at the same time rearranging the tissue in one or both breasts for a better cosmetic result. Is this something I am a candidate for?
- If you/my surgeon uses the Oncoplastic Lumpectomy technique, will I need a plastic surgeon? If so, how will this work? Will I select the plastic surgeon?
- Will you do a sentinel node biopsy to identify lymph node involvement? How will you tell how many lymph nodes are involved? Will you need to take more than the sentinel lymph node in my case? Are there circumstances that warrant removal of all the lymph nodes under my arm? (“axillary lymph node dissection”)
- What techniques do you use to locate cancerous lymph nodes?
- Do you recommend radiation after the lumpectomy to take care of residual disease?
- If you are recommending a mastectomy, can you explain why? Will it improve my survival?
- I have been diagnosed with ILC in one breast. I know imaging sometimes misses the presence of ILC in the other breast. Do you recommend a bilateral mastectomy (removing the opposite breast)? Why or why not? Will removal of the other breast decrease recurrence of lobular breast cancer? Can I elect a bilateral mastectomy even if you do not recommend it
- What is the risk to developing cancer in my opposite breast due to my ILC diagnosis if it is not removed?
- Can you do a nipple sparing mastectomy? Is there any risk in lobular cancer that the nipple may be involved with the cancer? Will I have any sensation in my breasts or nipples after skin/nipple sparing surgery?
- What are my options if I choose to have breast reconstruction? Do you coordinate surgery with a plastic surgeon? Do you recommend flap reconstruction, implants, or intraoperative reconstruction during surgery? Or aesthetic flat closure? Can you explain the pros and cons of each and the reason for your recommendation?
- What is the difference in recovery time for mastectomy with and without reconstruction? How many surgeries will I need if I choose implants? If I choose flap? If I choose nothing?
- Can you show me photos of what my chest may look like if I am deciding about getting reconstruction?
- If I have multiple tumors in one breast or in both breasts, what surgery would you recommend?
- If I have LCIS (Lobular Carcinoma in Situ) or DCIS (Ductal Carcinoma in Situ), will you recommend surgery?
- Are there any surgical clinical trials that I may be a candidate for? Are any of them specific for lobular breast cancer?
- If I have a mastectomy, will I have to have drains put in? For how long?
- Will the surgery be outpatient or inpatient?
- How long will my recovery be from a mastectomy? From a lumpectomy?
- Will you prescribe pain medications?
- Who will follow up with me about my recovery?
- Am I at risk of getting lymphedema or cording after surgery?
- How will I recognize if I have lymphedema or cording? Are there any precautions I can take?
- What can I do to ensure that I get back full motion of my arm(s) after surgery? Do you recommend breast physical therapy or lymphedema massage? Does this recommendation differ depending on the kind of surgery I have? Can you refer me for this care?
- Do you recommend radiation and when?
- Do I have dense breasts? Will you consider this when you order future scans? Are there any guidelines for imaging tests or timelines for follow up if I have dense breasts?
- If your recommendation is radiation therapy, what type of radiation are you recommending? External Beam- Whole breast or Partial radiation? Hypofractionated radiation? Can you explain the differences and why you recommend the one you do?
- Can you explain how radiation reduces the risk of recurrence?
- Do I need radiation to the axillary lymph nodes? Why or why not? Will radiation to this area improve my survival or decrease risk of local recurrence? What effect will the radiation have on my risk of developing lymphedema?
- Under what circumstances might I need radiation to my chest wall area (the supraclavicular or infraclavicular nodes)?
- If I need it, is there a particular type and number of treatments?
- Will I need a “boost” dose of my radiation treatment, can you explain what is it, when will I receive it, and why I need it?
- What are the risks and side effects of radiation? What can be done to minimize these side effects?
- What techniques are used to protect my heart if cancer is in left breast?
- What is the best sequence for radiation with implants? Are there risks to doing radiation after having implants? Can I have radiation with expanders and then implants?
- What type of imaging will you order if I have any signs or symptoms of a recurrence in these areas?
- If a biopsy confirms a recurrence is in my breast, do you recommend another surgery? What type?
- If I choose a lumpectomy, will I be able to have radiation if I have had it previously in the same breast?
- If the recurrence is in my lymph nodes, will you recommend surgery?
- Is it possible to treat the lymph nodes with radiation only?
- Do you have any integrative services? If not, can you recommend any in my area?
- Do you have a nurse practitioner or pain management team to help with my symptoms or side effects?
- Do you have any yoga, exercise, or meditation classes?
- Do you offer any psycho-social support or support groups for me or my family members in your clinic or that you can recommend in my area?
- Do you have any survivorship programs, financial planning, or other education programs?
- How is information regarding my treatment and follow-up communicated with my PCP (primary care physician), general practitioner, or family doctor?
- If I have a concern which may be related to breast cancer or treatment, who do I contact first? My primary care physician or my oncologist?
- Do you have a clinical trial coordinator in your institution that can help identify potential trials for me?
- When would be the best time for me to consider a Clinical Trial? What would be the benefits or drawbacks of enrolling in a clinical trial at this time?
- What clinical trials in your institution or in nearby institutions are available to me at this time?
- What are the options for clinical trials if I am willing to travel?
- Are there any clinical trials that are available for my specific mutation even if it is not a breast cancer specific trial?
- Are there any lobular specific trials available to me?
Section 2: Questions if You Have Been Diagnosed with Metastatic Lobular Breast Cancer (either recurrent or identified at initial diagnosis as “de-novo metastatic”)
- Are you a breast cancer specialist?
- How many patients with metastatic breast cancer do you treat?
- How many of them have lobular breast cancer?
- Who else will be on my care team?
- Will you treat me any differently due to my lobular breast cancer diagnosis?
- How will you follow my response to treatment?
- Are you comfortable with me seeking a second opinion if I choose to do so?
- How often will I have to come into the clinic?
- Are you familiar with ongoing research in metastatic lobular breast cancer? Are you open to receiving new studies or research I may come across?
- Do you have any special programs or groups for metastatic patients?
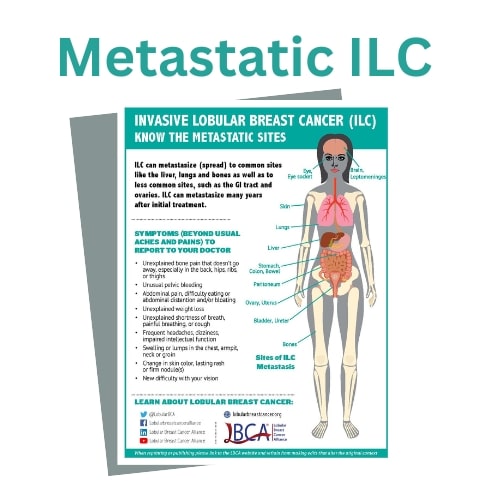
- Where has the cancer spread?
- Which type of scans visualized the spread of my cancer? How accurate is the imaging in detecting lobular breast cancer in all the locations the cancer can metastasize or has metastasized to? Are there additional imaging tests that can be done to verify the extent of the cancer?
- Will I need a biopsy? What areas? What are the risks and side effects involved? If it is an area that is not easily biopsied, what other approaches or tests can you order?
- If the cancer is also in my breast – will there be any reason for breast surgery in the future?
- If I am considered oligometastatic (i.e., meaning I have only a few new tumors in only one or two other parts of my body), will I be a candidate for treatment with “curative intent”? What treatments might this involve: chemotherapy, radiation and/or systemic treatment? What will be the order?
- If recurrent, has the subtype changed from the original cancer? What are the differences?
- How aggressive is the cancer? How will this affect my prognosis?
- Is the tumor HER2 low?
- Can you explain the entire report and what the various measurements/percentages will now mean for my treatment?
- Which type of imaging is better for the area(s) of metastases? CT Scan, PET scan, Bone Scan? Or all three? How often will I need them?
- Which scans or tests can see unusual sites of lobular breast cancer such as in the abdomen, GI (Gastrointestinal) tract or brain?
- Should I get a brain MRI?
- What is an FES/PET scan? Is it a type of imaging that will help in monitoring my metastasis?
- What can I expect to learn from the scan results and how might this information affect my treatment plan?
- Is it possible for you to alert the radiologist of my lobular diagnosis so that he/she is looking for radiologic
signs of metastasis from my lobular cancer?
- Are there tests you will order on the metastatic tumor specimen that will give you information that will help you determine the therapy you recommend for me? Why are these tests the most helpful? Will they cost me anything?
- Do you recommend that I have genetic counseling? If so, where would I get this?
- Are there other tests (like blood tests or additional biopsies) that you will use to track my cancer? Which ones, how often, and what will you be looking for?
- If the cancer is ER+, what treatment will you recommend? If I was previously on Tamoxifen or an Aromatase inhibitor, which one will you put me on now?
- Do you also recommend adding a CDK 4/6 inhibitor (targeted therapy) to the hormone regimen? Does the CDK 4/6 inhibitor improve the response to the hormonal treatment?
- Which CDK 4/6 inhibitor are you recommending and why?
- If the subtype has changed or I have targetable mutations, what treatment will you recommend?
- If you are recommending chemotherapy – Which one and why?
- What are the side effects of the treatment you are recommending? What can you do for neutropenia (low white blood cell counts), GI issues, mouth sores, etc.?
- Are you willing to lower the dose if the side effects are intolerable? Do I need to start at the highest recommended dose or is it possible to start at the lowest effective dose?
- How often will I be monitored?
- What are the pros and cons of having breast surgery since I already have metastatic cancer?
- If I choose to do surgery, which type of surgery do you recommend based on my metastatic diagnosis and previous surgical history?
- What are the risks and/or benefits in having a mastectomy based on my diagnosis and area of metastasis?
- If I have already had a lumpectomy, can I have another surgery in the same breast?
- Is there a survival benefit in doing surgery my case?
- Will you order genomic testing to determine if the tumor has specific mutations that can be targeted? Is there a PIK3CA mutation? Is the tumor mutational burden high?
- Is the subtype still the same? If not, what treatments will you recommend?
- Are there targeted therapies available for my subtype?
- What drugs and in what order will you recommend me taking them if my cancer progresses?
- Will I need chemotherapy? Which one and why? Are there oral chemotherapies that I can take before I would need IV chemotherapy?
- Will you be testing tumor markers? If so, which ones?
- Is there a clinical trial available for my tumor type?
- Do you have palliative care (supportive care) services? Any integrative services? If not, can you recommend any in my area?
- Do you have a nurse practitioner or pain management team to help with my symptoms or side effects?
- Do you have any yoga, exercise, meditation classes, support groups, or psycho-social support in your clinic for me and/or my family or that you can recommend in my area?
- Do you have any survivorship programs, financial planning, hospice, and end of life education programs?
- Do you have a clinical trial coordinator in your institution that can help identify potential trials for me?
- When would the best time for me to consider a clinical trial? What would be the benefits or drawbacks of enrolling in a clinical trial at this time?
- What clinical trials in your institution or in nearby institutions are available to me at this time?
- What are the options for clinical trials if I am willing to travel?
- Are there any clinical trials that are available for specific mutations in my cancer even if it is not a breast cancer specific trial?
- Are there any lobular specific trials available to me?
- Where are the bone metastases? Will you review my scans with me and show me where they are?
- What imaging is best to track metastases in my bones?
- How often will I have to have scans? Should I be concerned about exposure to radiation from my scans? How much radiation will I receive from each scan and what is the risk from this dose?
- Is there a benefit in ordering a biopsy in my bones? Are the sites in a safely accessible place for biopsying and what are the risks? Is there enough tissue to remove for a successful biopsy?
- What is the difference between lytic and sclerotic lesions? Will they heal?
- Is there a risk of fracture in any area? What can I do to help prevent a bone fracture?
- If I have bone pain, will you recommend radiation to help? What other methods will you recommend?
- Will you recommend bisphosphonates to prevent skeletal events? What are the benefits or risks of these drugs? What are the side effects? What are the risks of ONJ (osteonecrosis of the jaw) or hip fractures due to this medication? Would a “drug holiday” or something else lower these risks?
- Will it be administered by infusions or injections? How often and for what duration?
- Should I have any dental work completed before hand and stop the treatment before any dental work?
- Will you recommend radiation? What is the intention?
- How long will I need radiation? What are the side effects? What can I do to minimize the side effects?
- Will the radiation help with bone pain?
- How often can the bones be radiated? Is there a danger to my bone marrow if they are radiated several times?
- If there are skull metastases, will that put me at increased risk for brain metastasis? Will I need radiation to my skull?
- How many metastases do I have in my liver? Will you recommend a biopsy of my liver?
- What blood tests or scans are best for my liver metastasis?
- Is there a circumstance in which I would need to see a liver specialist?
- How does the liver metastasis impact my treatment options?
- How much has it impacted my liver function? What can I do if my liver function is compromised?
- What kind of dietary restrictions or lifestyle changes should I do to help with liver function?
- Can my lung tumor or nodule be biopsied? What are the risks?
- Will I need to see a Pulmonologist?
- How will the pathology affect my treatment options?
- What specific modalities/techniques will help with the impact of lung metastases?
- Is there fluid in my lungs? Will it have to be drained? Should I have a catheter placed? Will I be referred to a thoracic surgeon?
- How would you determine if I needed to be put on oxygen?
- Which scans or procedures show the metastases?
- What are the symptoms of progression to the GI tract, and can they be seen in a scan?
- If I have symptoms but nothing is seen on scans, which additional tests can be done?
- Will you do a biopsy? Can you biopsy all of the areas?
- Will I need to see a Gastroenterologist for a colonoscopy or endoscopy?
- Under what circumstances would I need laparoscopy (surgical procedure)? Will I need to see a Gastroenterology surgeon?
- What treatment do you recommend if I have fluid (ascites) in my abdomen?
- Will the pathology results help you determine my best treatment options?
- What other modalities, dietary or lifestyle changes can help me with this?
- What scan shows that there is metastasis in my brain? Do I need an MRI?
- What did the MRI show?
- Do you recommend a radiation oncologist and/or neuro-oncologist that specializes in brain metastases?
- Is there metastasis in the brain or in the leptomeninges (tissue lining)?
- Will I need radiation? And what type of radiation will give me the best control of my brain metastasis while minimizing the side effects to my brain function? What are the side effects?
- If the is cancer is in my eye area, will radiation help? What type of radiation is used? What effect will radiation in this area have on my vision?
- Will I need chemotherapy if I am not already on it? Will you change the chemotherapy if I am?
- What treatments are available for leptomeningeal metastases?
- Will you biopsy the skin metastasis?
- Can it/they be removed?
- Will I need any imaging done? What kind?
- Is there a special type of treatment for skin metastases or will it just be treated systemically? If so, will it be Chemotherapy, Radiation, Electrochemotherapy, or topical treatments?
- What kind of side effects can I expect from the treatment?
LBCA seeks to be the go-to source of up-to-date, research-based information, specific to lobular breast disease. LBCA does not wish to re-create resources that are valuable and accessible from other breast cancer resource organizations. The following websites have glossaries that can be useful in learning about terms and basic vocabulary used throughout the diagnosis, treatment, and monitoring of breast cancer:
- Komen (Breast Cancer Glossary): https://www.komen.org/support-resources/tools/glossary/
- American Cancer Society (Cancer Glossary): https://www.cancer.org/cancer/glossary.html
- Cancer.gov (website of NCI part of NIH): https://www.cancer.gov/types/breast/patient/breast-treatment-pdq
- NCCN Patient Guide: https://www.nccn.org/patients/guidelines/content/PDF/breast-invasive-patient.pdf or https://www.nccn.org/patients/guidelines/content/PDF/stage_iv_breast-patient.pdf
In preparing for an appointment with any of your cancer specialists or team, we recommend:
- You ask for, receive, and review any test results, pathology, surgical, and radiology reports, and doctor’s notes that may be available.
- If you have any questions about anything in these results including what they may suggest about your diagnosis, prognosis, or advisable course of treatment, write these questions down and bring them with you to your meeting with your doctors.
- Reviewing them on your own beforehand can help you discover questions that had not occurred to you or about which you now seek additional clarification.
- Bring someone with you when you consult with a doctor who can take notes.
- If not possible, you may wish to use your phone to record the conversation or invite a friend or family member to listen to the visit via phone to enable them to take notes.