ILC Facts
Facts About Invasive Lobular Carcinoma: A Distinct Subtype of Breast Cancer
The following information about invasive lobular carcinoma (ILC), also known as lobular breast cancer, is for informational and educational purposes only to assist patients and caregivers with learning about ILC. The information is not meant to replace the advice and information patients receive from their health care providers. Learn more about ILC by reading LBCA’s Frequently Asked Questions.
View and download the ILC Fact Sheet in other languages:
(Published 2018; Updated 2/7/2023)
If you don’t see an ILC Fact Sheet in your desired language, we invite you to visit the European Lobular Breast Cancer Consortium (ELBCC) Leaflet page to see if they have information in that language. The ELBCC closely collaborates with LBCA. All the information they share is also fact checked and peer reviewed by researchers, clinicians, and patients.
Lobular breast cancer is not a “rare” cancer.
Lobular breast cancer, also known as invasive lobular carcinoma (ILC), is the second most common histological type of breast cancer diagnosed, accounting for about 10-15% of all breast cancers. [1],[2] An estimated 43,000 new cases of ILC are diagnosed each year. ILC impacts more women than do cancers of the kidney, brain, pancreas, liver, or ovaries.[3]
Lobular breast cancer is a distinct subtype of breast cancer.
A hallmark of the most common type of ILC is the absence of the protein E-cadherin. [2] ILC also has unique subtypes and variants. [1] It is evident that the clinical behavior and molecular features of ILC are distinct from the most common type of breast cancer, invasive ductal cancer (IDC), also known as IDC/NST (No Special Type).[1],[2],[4] More research is needed to better understand ILC’s biology and behaviors to identify ILC-specific therapies.
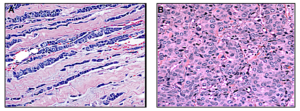
ILC cells (on the left) form a distinct, single-file pattern that is very different from the more common ductal breast cancer cells (on the right).
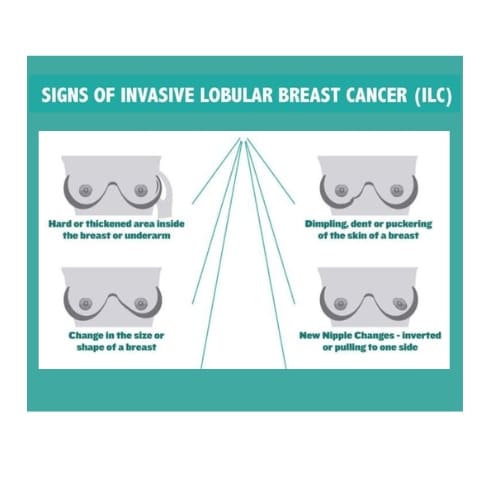
Lobular breast cancer tumors do not usually form in lumps and are hard to feel in self-exams.
In most cases, ILC tumors form in threadlike patterns rather than lumps. This can make even large ILC tumors hard to feel.
Symptoms of ILC tumors can range from none to changes in the appearance of the nipple or breast, such as dimpling, hardening of the breast, swelling, or pain. [4],[5] On self-examination, ILC can sometimes be felt as a firmness or mass.
Know the signs and symptoms of lobular breast cancer.

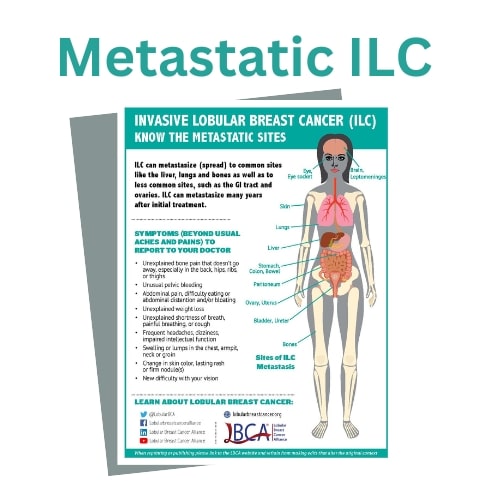
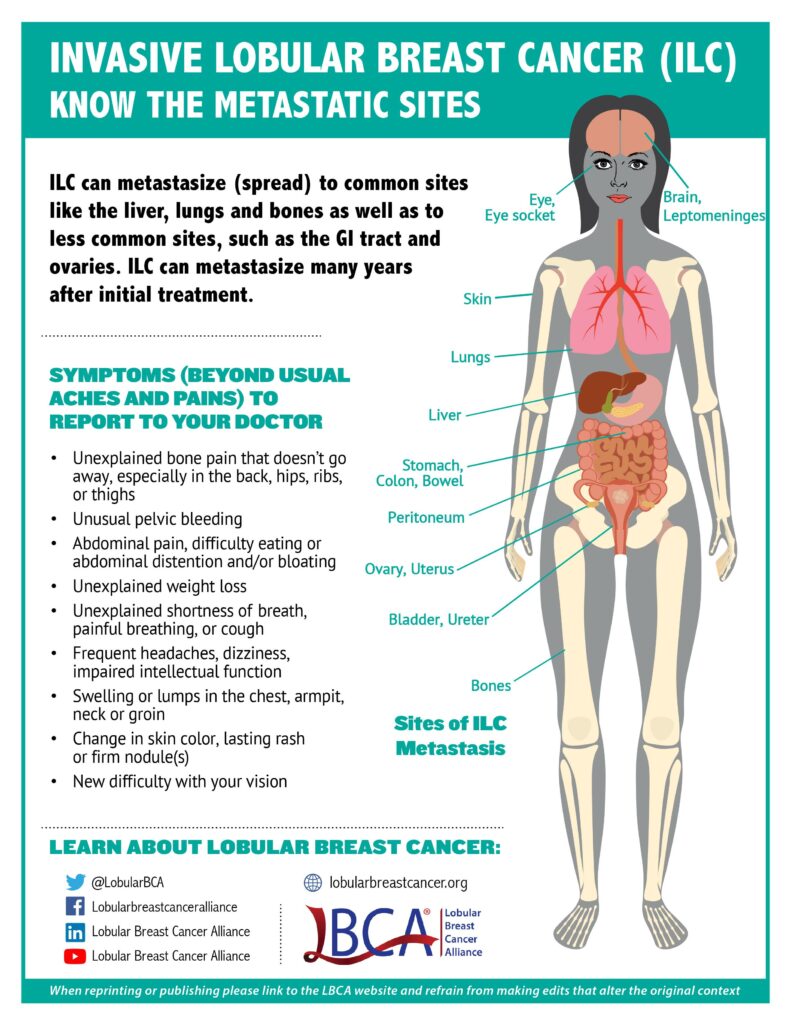
Lobular breast cancer can metastasize to unusual places.
Similar to IDC/NST, ILC can metastasize to the bones, brain, liver, and lungs. However, ILC can also spread to unique sites such as the gastrointestinal tract (stomach, small intestine, and colon), gynecological organs (ovaries, uterus), the peritoneum (abdominal lining), and in rarer cases leptomeninges (lining of the brain and spinal cord) [6] and orbital tissues (tissues around the eye). [7] A printable pdf of the sites and symptoms of metastatic breast cancer is available.
Lobular breast tumors frequently recur many years after primary diagnosis.
While lobular breast cancer, like IDC/NST, can recur any time after initial diagnosis, studies show that ILC often recurs later than IDC, more than 10 years after the initial diagnosis of cancer. [8]
Lobular breast cancer is harder to detect in screening and advanced imaging.
Since ILC typically grows in a linear pattern through the breast without distorting the surrounding structures or forming a lump, ILC is more difficult to detect than IDC on mammography and ultrasound or to visualize when metastatic. ILC is often missed in routine screening resulting in larger and later stage tumors when detected and diagnosed. Screening mammograms are still important as they can identify lobular breast cancers as well as other types of breast carcinomas.
Lobular breast cancer is currently treated like the more common IDC/NST despite its differences.
An individual’s treatment plan for ILC depends on many factors, including the size and grade of the cancer, genetic factors, lymphnode involvement, and the patient’s overall health and individual preferences. At present, there are no ILC-specific treatment guidelines. The standard of care for early-stage treatment of hormone receptor positive ILC is the same as treatment of hormone receptor positive IDC/NST. More research is needed to identify ILC-specific treatment protocols. [9]
[1] McCart Reed AE, et al. Invasive lobular carcinoma of the breast: the increasing importance of this special subtype. Breast Cancer Res. 2021 Jan 7;23(1):6. PMID: 33413533
[2] Ciriello G, et al. Comprehensive Molecular Portraits of Invasive Lobular Breast Cancer. Cell. 2015 Oct 8;163(2):506-19. PMID: 26451490
[3] 2021 Projected Incidence from ACS Surveillance Research (Source: SEER data)
[4] Wilson N, et al. Lobular Breast Cancer: A Review. Front Oncol. 2021 Jan 15;10 PMID: 33520704
[5] https://lobularbreastcancer.org/wp-content/uploads/2022/10/Symptoms_of_ILC_2022.pdf
[6] Franzoi MA, et al. Leptomeningeal carcinomatosis in patients with breast cancer. Crit Rev Oncol Hematol. 2019 Mar;135:85-94. PMID: 30819451
[7] Blohmer M, et al. Patient treatment and outcome after breast cancer orbital and periorbital metastases: a comprehensive case series including analysis of lobular versus ductal tumor histology. Breast Cancer Res. 2020 Jun 26;22(1):70. PMID: 32586354
[8] Pestalozzi BC, et al. International Breast Cancer Study Group. Distinct clinical and prognostic features of infiltrating lobular carcinoma of the breast: combined results of 15 International Breast Cancer Study Group clinical trials. J Clin Oncol. 2008 Jun 20;26(18):3006-14. PMID: 18458044
[9] Oesterreich S, et al. Clinicopathological Features and Outcomes Comparing Patients With Invasive Ductal and
Lobular Breast Cancer, J National Cancer Institute, 2022 Nov 114:11: 1511-22, https://doi.org/10.1093/jnci/djac157