Metastatic ILC Information
Learn About Metastatic ILC
The information and materials provided here were compiled for use by people with metastatic invasive lobular carcinoma (ILC) and others with ILC that seek to learn more.
ILC can metastasize many years after initial diagnosis. Because of ILC’s unique features there may be challenges in diagnosis, and differences in imaging, treatment, and clinical trials. LBCA hopes the provided information may be used by individuals to better understand the nuances of metastatic ILC and that it will be helpful in discussions with care teams.
LBCA strives to keep this page current as new information and research findings become available.
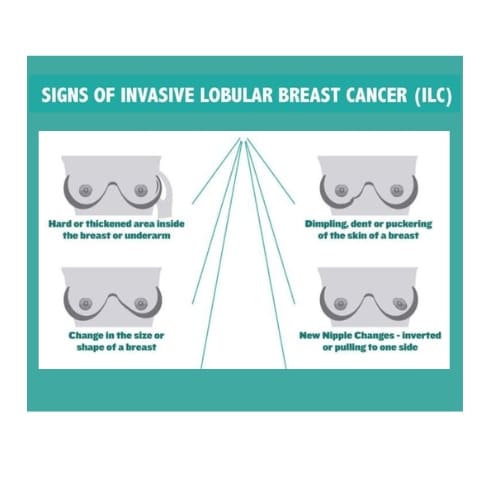
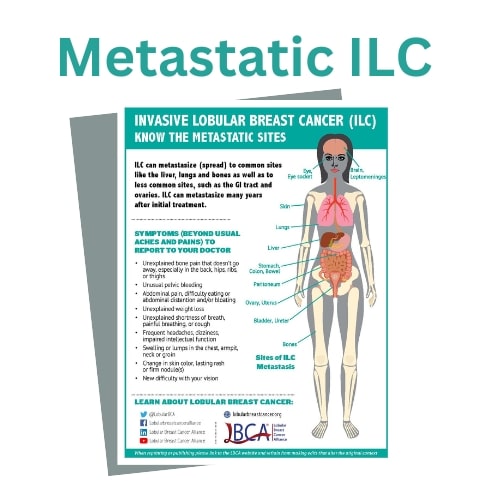
Sites and Symptoms of Metastatic Breast Cancer
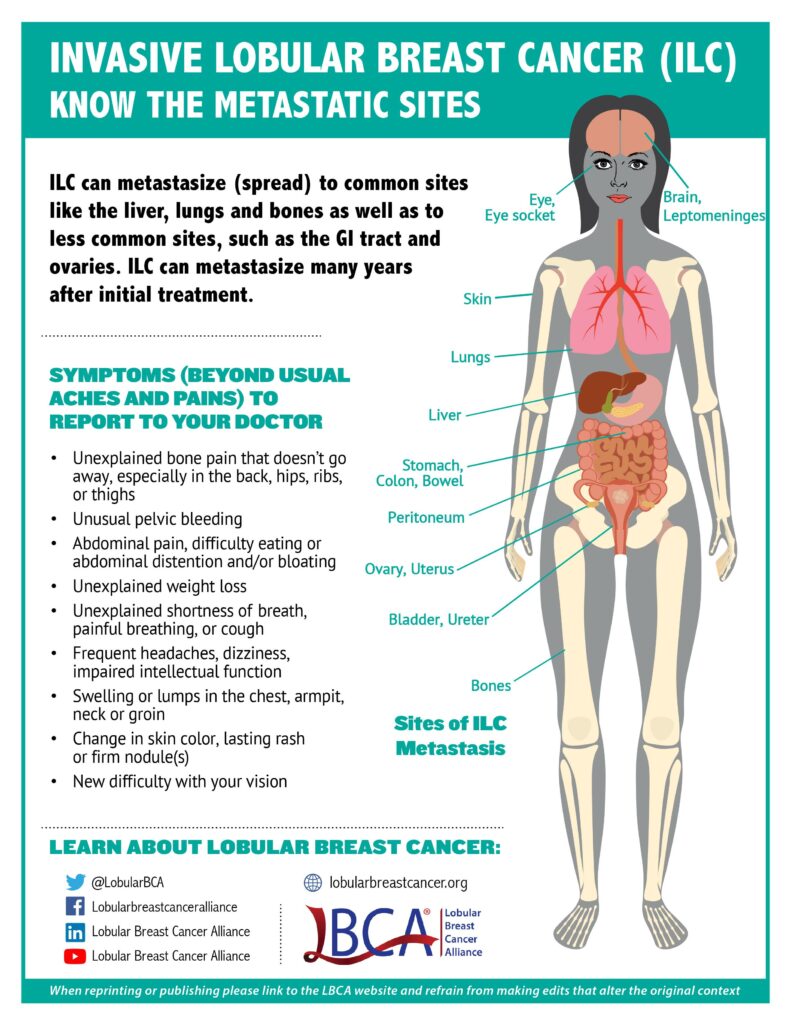
If you have been diagnosed with lobular breast cancer, it’s important to know where lobular breast cancer can metastasize (spread) and the symptoms. Like invasive ductal carcinoma (IDC), ILC can metastasize to the bones, lungs, liver, thoracic and abdominal lymph nodes, and brain, but can also spread to unusual sites such as the gastrointestinal tract (i.e., stomach, small intestine, colon), reproductive organs (i.e., ovaries, uterus), the abdominal lining (i.e., peritoneum), and the genito-urinary system (i.e., bladder and ureter).
As with IDC, the most common site of ILC metastases is to the bones. Lung and liver may be less common sites for metastases in ILC than in IDC. However, ILC may travel to tissues such as the pleura (lining of the lung) and in rarer cases, the leptomeninges (lining of the brain and spinal cord) and the orbital canal (tissues behind the eye).
Because of the potential for ILC to metastasize to uncommon sites, it is important for people with lobular breast cancer and their oncologists to be aware of these differences, and to discuss the importance of recognizing and reporting possible symptoms referring to these unusual sites of metastases.
View and download the Metastatic ILC Graphic in other languages:
Metastatic ILC Imaging
The linear growth pattern of ILC sometimes makes it difficult to detect metastatic ILC with current imaging technology such as traditional computed tomography (CT), positron emission tomography (PET) and bone scans. It is well established that primary ILC (in the breast) can be more difficult to detect on imaging than primary IDC. Distant metastases in all breast cancers are more easily seen in the bones, liver, and lungs than in other unusual sites. However, studies are showing that certain types of imaging may be more effective in visualizing different sites of ILC metastases. For example, bone metastases (the most common site of ILC metastases) may be more visible on integrated FDG PET/CT scans than on CT/bone scans. There is quite a bit of variety in the efficacy of the types of scans used in relation to different sites of metastases suspected. This makes it extremely important for radiologists to be aware of the ILC histologic subtype when interpreting imaging scans for metastatic disease, and it is also important to note what has proven to work well in each individual patient.
Current research on new types of PET scans are showing promise in ILC. Two early prospective trials on new imaging tracers for PET scans are demonstrating value at imaging ILC, with some advantages compared to the currently available FDG PET, which targets sugar metabolism. Fluoroestradiol (FES) is a novel imaging tracer (recently FDA approved), based on estrogen expression in ER+ tumors and may also more reliably assess anti-estrogen therapy response than FDG PET/CT. Fluciclovine (FACBC) targets amino acid metabolism and may also more accurately detect ILC metastases than other imaging methods.
These new tracers could provide improved evaluation of metastases and assessment of treatment responses and could therefore result in improved treatment decisions for patients with ILC. Learn more by reading FDG and Non-FDG Radiopharmaceuticals for PET Imaging in Invasive Lobular Breast Carcinoma and our scientific blog by LBCA Scientific Advisor Dr. Gary Ulaner.
Clinical Trials

One of the primary challenges with studying treatment effect is that the typical mechanism used to assess efficacy in clinical trials with metastatic patients, the RECIST criteria, measures treatment response on CT scan based on “measurable” disease, which is less common in ILC. Due to the diffuse pattern of ILC, it often does not form a mass, making it “unmeasurable,” therefore making these patients ineligible for many trials. In a recent abstract, patients with metastatic ILC were shown to be significantly underrepresented in clinical trials of breast cancer, likely due to the application of RECIST criteria.
Improved staging and/or detection of disease/disease recurrence could result in improved treatment in patients with metastatic ILC. There are current and prospective clinical trials that are using new types of tracers for imaging showing promise in visualizing ILC. There is also potential for using a different criteria called PERCIST, using PET scans for assessing treatment response. These new methods will potentially enable more patients with metastatic ILC to be eligible for clinical trials.
A second key challenge in conducting clinical trials that include a metastatic ILC cohort is that it is frequently harder to find and enroll a sufficient number of patients with ILC. This is because of the relatively lower percentage of patients with ILC as compared to IDC. It is important for more lobular-specific and multicenter trials that include lobular cohorts to increase the numbers of lobular patients. Trials that measure treatment efficacy in ILC will in turn result in more clinical trials being open to patients with metastatic ILC.
Learn more about existing lobular-specific and lobular-enriched clinical trials.
Metastatic Trial Search is an easy-to-use clinical trial matching service developed specifically to meet the needs of people with advanced and metastatic breast cancer. With this service you can match to trials based on breast cancer subtype, including lobular; sites of lobular-specific metastases, biomarkers, and more. Users can view important trial information in a patient-friendly format. Metastatic Trial Search is designed to be used by patients, caregivers, navigators and healthcare providers. Metastatic Trial Search is now improved with the addition of 10 tutorial videos and accompanying written guides located throughout the site. You can browse trials as a guest or create a profile.
Biomarkers and Inherited Mutations

While genetic (or germline hereditary) mutations in certain genes can increase the risk of developing breast cancer, tumors themselves can also acquire genomic mutations that can act as treatment targets. Hereditary mutations in CDH1 can confer a lifetime risk of both ILC and Hereditary Diffuse Gastric Cancer (HDGC). Patients with ILC can also have hereditary mutations in other genes including BRCA2, CHEK2, and PALB2. Currently there are treatments targeting BRCA mutations (PARP Inhibitors) available for patients with metastatic ILC.
Biomarker testing in tissue or liquid biopsy may be useful in identifying genomic mutations that have approved drugs or are being studied in clinical trials. Many ILC tumors harbor a genomic CDH1 mutation for which there is currently no targeted treatment. There are, however, other genomic mutations that are highly prevalent in lobular tumors, that do have targeted treatments or for which targeted treatments are being studied. For example, approximately 35-50% of lobular tumors harbor the PI3KCA mutation for which there is an approved targeted treatment; Apelisib (Piqray) for ER+ metastatic patients. Approximately 5-15% of lobular tumors harbor ERBB2 mutations, which occur in the HER2 pathway. Neratinib (an approved drug for HER2+ breast cancers) is being studied for efficacy of treatment in Metastatic ER+ breast cancers with a lobular cohort in an ongoing clinical trial.
Biomarker testing may also be useful in determining anti-estrogen resistance such as the finding of ESR1 mutations, and other mutations such as RB1, which may confer resistance to CDK 4/6 inhibitors. In other studies, ILC metastases are showing a higher TMB (tumor mutational burden) score relative to IDC. A TMB score is the number of mutations in a tumor and is used as a biomarker to help determine whether the tumor might respond to treatment with Immune Checkpoint Inhibitors (Immunotherapy).
Other genomic mutations that are prevalent in ILC including FOXA1, AKT1, PTEN, HER2, HER3, ATM, and FGFR mutations are currently being studied in the lab with the expectation that additional targets for treatment may emerge.
Because of the growing understanding about different biomarkers and what they may mean for future treatment for patients with metastatic ILC, it is increasingly common that biopsy of new metastatic sites, biomarker testing conducted either by tissue or liquid biopsy be considered. These tests are done with the hope that they will identify mutations for which there are currently targeted treatments or for which it is expected that there will be in the future.
Learn more about biomarker (genomic) testing in metastatic lobular breast cancer and the genomic characterization of stromal tumor-infiltrating lymphocytes and genomic alterations in metastatic lobular breast cancer.
Additional Metastatic ILC Resources
Virtual Meetup
Breastcancer.org and the Lobular Breast Cancer Alliance have collaborated on a monthly virtual meetup for those diagnosed with metastatic lobular breast cancer as a place to share and support. Hosted via Zoom, register for the next session here.
FAQs
MBCBrainMets.org
MBCBrainMets.org, a website hosted by SHARE Cancer Support, is an education and resource hub for metastatic breast cancer patients living with brain or leptomeningeal metastases, and their caregivers. It is a place where users can access unbiased expert educational resources, read stories for building community and hope, and be connected to the tools that can assist them in finding better outcomes.
Metastatic Breast Cancer Project
The Metastatic Breast Cancer Project is a nationwide movement of patients, doctors, and scientists working with metastatic breast cancer patients and advocacy organizations. Metastatic breast cancer patients, including those with metastatic lobular breast cancer, participate by sharing their tumor samples, their medical information, and their voice. The goal is to work together to speed the development of future therapies. A goal of the Metastatic Breast Cancer Project is to enable scientific discoveries and the development of new treatment strategies for metastatic breast cancer by widely sharing clinical, genomic, molecular, and patient-reported data.
Metastatic Breast Cancer Alliance and the Here All Year Campaign
The Lobular Breast Cancer Alliance is a member of the Metastatic Breast Cancer Alliance, and collaborated with the organization for its Here All Year Campaign in July, 2021. You will find topics from this campaign incorporated into the information on this page. View videos created by people with metastatic lobular breast cancer.
Metastatic ILC Poster
- In June 2022, LBCA conducted an online survey of individuals diagnosed with metastatic ILC to hear about their experiences living with metastatic lobular breast disease. The results were presented in an abstract and a poster at the San Antonio Breast Cancer Symposium (SABCS).
Metastatic Trial Talk
Metastatic Trial Talk (MTT) was created to address the overwhelming amount of breast cancer information available online. They carefully select news and features about metastatic breast cancer research to help patients when making treatment decisions, including whether to enter a clinical trial. MTT was developed by BreastCancerTrials.org as a companion to Metastatic Trial Search, a clinical trial matching tool designed specifically for people with metastatic breast cancer.
In September 2022, MTT share information focused on metastatic lobular breast cancer.
Metavivor.org
METAvivor has educational materials on research and awareness and peer-to-peer support for metastatic breast cancer patients.
Project Life
Project Life is a free virtual membership-based wellness house serving those living with stage IV advanced metastatic breast cancer as well as their caregivers. Their focus is on quality of life through five dimensions of wellness: financial, emotional, physical, social and spiritual. They concentrate on the whole person, building community and are inclusive of all regardless of skin color, and gender identity.
The virtual wellness house is for metastatic patients and their loved ones. All of our programming is offered for free. Project Life also offers Peer to Peer Mentorship. The mentorship program matches mentees with trained peer mentors who have similar experiences and uniquely supports the mentors. There are a number of volunteers living with metastatic ILC who are available to mentor individuals with similar lived experience. If you are interested in finding a mentor, or exploring opportunities to be a mentor, please contact the Director of Mentorship, Abigail Johnston at mentorship@projectlifembc.com. Project Life was founded and created by those living with the disease. #livewellgrowtogether
Questions for My Doctor
LBCA prepared a document with questions to be used with various members of your care team or with someone from whom you may be seeking another opinion. In preparing the questions, we developed this resource with the input of patient advocate volunteers as well as clinicians on our Scientific Advisory Board (SAB). We have grouped these questions into categories so that you may read and/or print out all or only those most relevant for you. Questions in Section 1 pertain to individuals with all stages of ILC while Sections 2 and 3 pertain specifically to metastatic ILC.
Podcasts and Videos
There are educational videos and podcasts, ILC- focused topics from past conferences, and videos on ILC topics being discussed by our Scientific Advisory Board members and other ILC expert researchers available for viewing. The podcasts and videos below may be helpful to those with metastatic lobular breast cancer.
Podcasts
LBCA Scientific Advisory Board (SAB) member Dr. Jason Mouabbi discusses treatment outcomes for lobular breast cancer in a podcast from July 2022.
Our MBC Life hosted a podcast titled Newly Diagnosed with MBC: Tests, Terms, & Tips with Dr. Rebecca Shatsky.
LBCA Executive Director Laurie Hutcheson, and Founding SAB Chair Dr. Steffi Oesterreich, and Dr. Adrian V. Lee discuss why ILC is so hard to research and what looks promising for the future in an episode of the podcast Our MBC Life.