Lobular Breast Cancer can be more difficult to see on imaging and scans. It can be harder to detect on mammograms, resulting in later-stage diagnosis and may be harder to detect on advanced imaging once it spreads beyond the breast.(1)

Gary Ulaner, MD, PhD, FACNM, radiologist and ILC researcher at Memorial Sloan Kettering Cancer Center and member of the Lobular Breast Cancer Alliance (LBCA) Scientific Advisory Board, shared his expertise on imaging challenges and options for lobular breast cancer. The National Cancer Institute Dictionary of Cancer Terms may assist patients reading this article.
LBCA: Why is Lobular Breast Cancer more difficult to detect on Imaging?
Dr. Ulaner: Not all breast cancer is the same. There are several different histologic subtypes of breast cancer. Histology is the microscopic structure of tissues, as can be seen under a microscope. Differences in the microscopic structures give rise to differences in the larger breast cancer lesions.
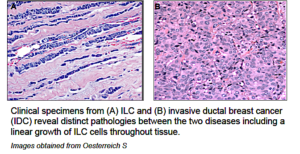 The most common histology of breast cancers is invasive ductal cancer (IDC). The second most common is invasive lobular cancer (ILC). ILC usually lacks a protein called E-cadherin which holds cells together. The loss of E-cadherin causes ILCs to grow as less compact masses, often as lines of cells through the fatty tissue of the breast. More compact masses are easier to see on radiology studies as they can be more easily seen as something different from normal tissue. The less compact growth of ILC makes it harder to see on radiology studies.
The most common histology of breast cancers is invasive ductal cancer (IDC). The second most common is invasive lobular cancer (ILC). ILC usually lacks a protein called E-cadherin which holds cells together. The loss of E-cadherin causes ILCs to grow as less compact masses, often as lines of cells through the fatty tissue of the breast. More compact masses are easier to see on radiology studies as they can be more easily seen as something different from normal tissue. The less compact growth of ILC makes it harder to see on radiology studies.
LBCA: What imaging is currently used in the breast?
Dr. Ulaner: Evaluation of local disease (disease in the breast) is usually done with mammography, ultrasound, and breast MRI. There are no histology-specific guidelines for screening, pre-operative in-breast staging, or evaluation of recurrent in-breast disease.
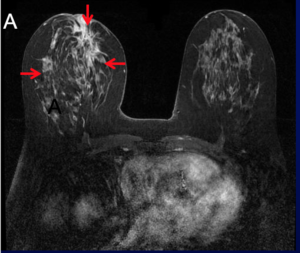
What is currently suggested for IDC is also followed for ILC, with radiologists realizing that it is harder to see ILC than IDC. MRI screening is utilized in patients with a high lifetime risk of breast cancer (>15%) as determined by family history, BRCA mutations, and other factors. MRI remains the most sensitive method of detecting disease within the breast; however, MRI has lower specificity than mammography and results in more biopsies.
LBCA: What kinds of breast imaging are currently being studied?
Dr. Ulaner: Additional methods of evaluating local disease include digital breast tomosynthesis (DBT), contrast-enhanced mammography CEM), breast-specific gamma imaging (BSGI), and positron emission mammography (PEM). These techniques are less widely available and are still being evaluated in clinical trials. Unfortunately, none of these techniques has yet demonstrated superior detection of ILC either. Extensive research on these methods are currently underway.
LBCA: How is lobular breast cancer currently imaged once it has spread outside of the breast?
Dr. Ulaner: Systemic staging for distant metastases (when cancer spreads to other parts of the body) is done with CT, bone scan, and PET/CT or PET/MRI. The current National Comprehensive Cancer Network (NCCN) guidelines do not have histology-specific advice for systemic staging. The current standard for systemic staging is CT with bone scan, although data is increasing that detection of distant metastases and evaluation of treatment response in distant metastases may be better performed by FDG PET/CT. Unfortunately, it is also harder to find distant metastases from ILC than from IDC.
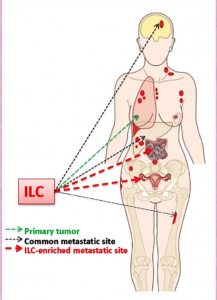
An important difference between ILC and IDC is their pattern of metastatic spread. While both IDC and ILC commonly metastasize to lymph nodes, bone and liver, ILC demonstrates a predilection for metastases to the peritoneum, retroperitoneum, and hollow viscera (including the gastrointestinal and genitourinary tracts). Lung metastases are more common in IDC.
“Knowledge of the histology of the breast cancer can help focus a radiologist’s attention to the areas of most common metastatic disease.”
LBCA: Please describe the different types of PET scans, and their potential use for ILC
Dr. Ulaner: With attention to PET/CT, there are several PET tracers (radioactive drugs) utilized, though the one currently used most frequently in the clinic is FDG.
- FDG (18F-fluorodeoxyglucose) is a sugar analogue. Cancers eat sugar and then can be seen on FDG PET scans. The FDG PET is performed with a CT or MR for multiple reasons, including characterizing the lesion found on FDG PET. FDG PET/CT has been successful at systemic staging of breast cancer and measuring treatment response. Like other imaging modalities, it is harder to see ILC than IDC on FDG PET.
- NaF (sodium 18F-floride) finds bone metastases. A NaF PET/CT is more sensitive for bone metastases than a typical “bone scan”, but also detects more benign findings, too, thus it is less commonly used.
- FES (18F-fluoroestradiol) is an estrogen analogue. It can find cancer that expresses estrogen receptor, and many breast cancers expression estrogen receptors, such as lobular breast cancer. FES is currently experimental and used in clinical trials.
- Axumin (18F-flucicloivne) is an amino acid analog. It is currently used in men with suspected recurrent prostate cancer. There is some evidence that ILC may take up more Axumin than FDG. Axumin is currently experimental and used in clinical trials.
LBCA: Which scan is best able to evaluate ILC based on where it has spread outside the breast (bones, abdomen, etc).
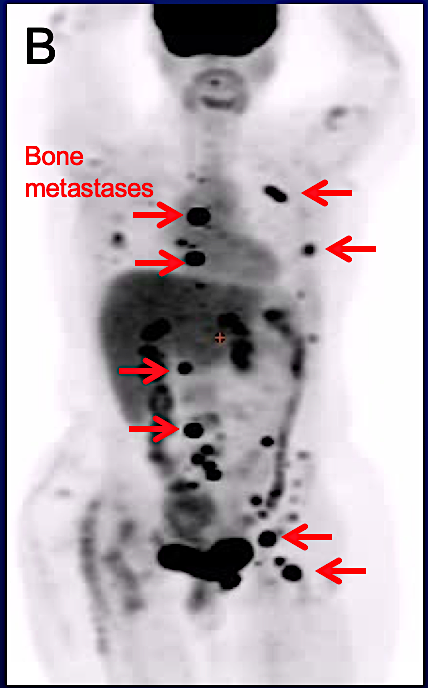
Dr. Ulaner: There is no one “best” answer for what imaging modalities are best for patients with ILC. If a patient has early stage disease (stage I or II), no systemic (full-body) imaging may be needed to look for metastasis. In locally advanced and metastatic ILC (stage 3 and 4), FDG PET/CT, CT, and/or bone scan may be used.
I like to say that every metastatic ILC deserves one chance at being FDG-avid (the ILC is visible on an FDG PET scan). If it is, FDG PET/CT is an excellent method for following extent of disease. If the metastatic ILC is not FDG-avid on an FDG PET/CT, then CT/bone scan is a better method.
LBCA: In your opinion, what might the future hold for imaging and ILC?
Dr. Ulaner: There are extensive on-going studies of breast cancer and it is difficult to predict which ones will become clinically important until the data is available. Importantly, researchers are now more aware of the differences between the histologies of breast cancer and are evaluating each histology more individually.
I believe digital breast tomosynthesis (DBT) will replace current mammography. Contrast enhanced mammography (CEM) will also likely be found to be more sensitive than current mammography and may be used in lieu of MRI in some patients. PET tracers targeted to estrogen receptor and human growth factor receptors may help select targeted therapies for patients with breast cancer. Biopsies, which are most commonly performed by ultrasound and mammogram guidance, will likely be commonly be performed by MRI and even PET guidance.
“It is a goal of many researchers to develop a method to image lobular breast cancer more sensitively than is currently available. I hope that goal will be achieved as soon as possible.”
– END –
Patients can ask their doctor to make sure their medical records and orders for all scans very clearly state “lobular breast cancer” and not just “breast cancer”. This can help the radiologist reading the image be aware of what to look for when evaluating imaging for both local and metastatic disease. If a patient is concerned about interpretation of their images, they can speak to their oncologists about requesting a second opinion from a National Cancer Institute (NCI) designated cancer center. NCI Designated Cancer Centers treat higher volumes of patients, see many more lobular cases, and have access to the latest research. It is always OK to request a second opinion on imaging.
(1) Johnson, K., Sarma, D. & Hwang, E.S. Lobular breast cancer series: imaging. Breast Cancer Res 17, 94 (2015),Hogan MP, Ulaner GA. J Nucl Med. 2015 Nov;56 (11):1674-80), American Journal of Roentgenology. 2014;202: 1140-1148. 10.2214/AJR.13.11156


